Optical coherence tomography (OCT) is an imaging technology that is often described as the optical equivalent to ultrasound. While this analogy is broadly correct, it does not convey the fact that OCT can do so much more than ultrasound. While it cannot penetrate as deeply into tissue as ultrasound, it has a higher resolution and can be combined with many other optical techniques to give a vast amount of information.
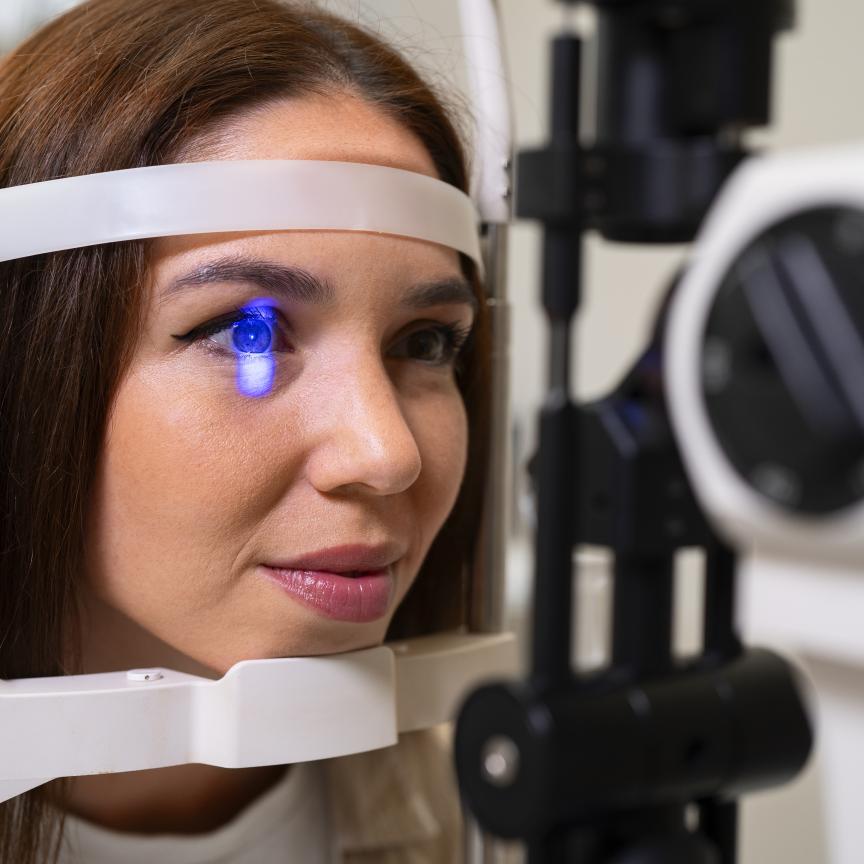
In ophthalmology, OCT can no longer be described as an ‘emerging’ technology – it is now accepted as a clinical standard for diagnosing and monitoring the treatment of a number of retinal diseases. OCT’s use in other medical areas has been limited by its poor penetration depth, which, in typical biological samples, is usually only a few millimetres. However, the development of endoscopic probes means OCT can be used to image hollow organs such as the gastrointestinal tract, the bladder and the heart. In cardiology, intravascular OCT can resolve significantly smaller details than the conventional technique of intravascular ultrasound. This makes OCT a valuable technique for visualising plaque lesions or checking the outcome of a stent deployment. The first commercial systems for intravascular OCT in cardiology have recently entered the market and intravascular OCT is now so mature that large-scale commercialisation is expected in the next few years.
OCT has also shown great promise in dermatology. Because skin is the most easily accessible part of the human body and OCT has a limited penetration depth, dermatology was one of the first applications investigated when OCT was first developed. However, the differentiation between benign and malignant lesions in a clinical setting is a huge challenge, because benign lesions often show the same structure in OCT images as malignant ones.
Adding functionality
It is in cases such as this where functional OCT could help. While OCT can reveal the morphology (thicknesses of different layers) of a sample, combining OCT with other techniques can reveal much more information. For example, polarisation-sensitive OCT can reveal the different structures of each layer; Doppler OCT can reveal blood flow in a sample; multiphoton tomography can add chemical specificity to the structural imaging capability of OCT; and combining OCT with photoacoustic tomography can give a detailed map of blood vessels – valuable for diagnosing tumours.
It is this idea of combining different techniques to create functional OCT that has been the focus of a pan-European research project for the last three years. Called FUN OCT, the project includes six partners from Denmark, Germany and Austria.
‘The aim of FUN OCT is to expand the non-invasive optical biopsy capability of OCT and combine it with multiphoton tomography to develop novel functional capabilities enabling “morphofunctional” performance,’ explains Peter Andersen, from the Technical University of Denmark, and FUN OCT coordinator. ‘These methodologies will enable unprecedented non-invasive detection of depth-resolved physiological, metabolic and molecular specific tissue information.’
FUN OCT consortium members have made considerable progress in a number of areas including polarisation-sensitive OCT, Doppler OCT and light source technology. However Andersen highlights two areas of the project that he thinks are particularly exciting. ‘Researchers at the Ludwig-Maximilians University (LMU) in Munich, Germany, have used a newly developed laser source – the Fourier-domain mode-locked (FDML) laser – to obtain amazing images of the eye,’ says Andersen. ‘Also, researchers in Austria have combined photoacoustic tomography with OCT to give high-resolution 3D imaging of vascular structures to depths of up to 5mm.’
A new laser source
The FDML laser was invented by Robert Huber while he was working with OCT pioneer James Fujimoto at the Massachusetts Institute of Technology. It is fundamentally different to standard tunable lasers. In an FDML laser the cavity length is increased up to several kilometres. Huber, who is now at the LMU in Munich, Germany, says: ‘We developed the FDML in order to overcome the tuning speed limitations of standard lasers. We use a semiconductor optical amplifier as our gain medium and a fibre spool is used to increase the cavity length. The challenge is to synchronise the optical round trip time with the tuning rate of the filter so that by the time light with a certain wavelength arrives back at the filter, the filter has been tuned over exactly one wavelength sweep.’
The FDML laser was developed for use in swept-source OCT, where each sweep of the laser generates one depth scan, or A-scan. Unlike other swept sources that are currently on the market, the sweep rate of the FDML laser is only limited by the speed of the filter and not by fundamental laser physics. This has enabled Huber and his colleagues to achieve sweep repetition rates of up to 5MHz, which makes this system more than 50 times faster than current commercial instruments.
‘Tuning speed in standard setups is limited by the time required to build up lasing from amplified spontaneous emission background at each new spectral position to which the laser is tuned,’ says Huber. ‘Our system is only limited by how fast we can drive the fibre Fabry-Perot tunable filter, which is used as the optical bandpass filter. It is really surprising that the filter can be controlled precisely enough so that it can be driven at such high speeds with sufficient repeatability for synchronisation. This enables us to almost perfectly synchronise the filter with the optical round trip time.’
But as Huber points out, there are many more challenges in this area of research than the technology alone. While the researchers have demonstrated unprecedented performance, it is debated in the industry as to whether this kind of speed is actually required. ‘The higher the speed, the less signal and the more complex the system,’ says Huber. ‘We have to demonstrate the benefits of high speed OCT clearly for different applications to enable a range of new commercial applications and markets.’
Ultra high speed OCT imaging has distinct advantages over lower speed systems. It allows transient dynamics to be resolved in real time and enables dense sampling of in vivo samples where OCT acquisition times are usually restricted to a few seconds due to motion. Using slower systems, OCT images are restricted to small areas or dense sampling is not possible. Dense sampling not only increases the amount of recorded information, but also allows for advanced averaging methods in post-processing. This is a considerable advantage over other averaging methods that require fixing of the averaging area prior to data acquisition.
‘We believe that FDML lasers offer better speed performance in the 1050nm, 1300nm and 1550nm wavelength range than line scan cameras or current commercially available short cavity swept lasers,’ says Huber. 1050nm light can be used for retinal imaging, because of the moderate water absorption in this wavelength range. 1300nm is the wavelength of choice for imaging in highly scattering tissue and is used for intravascular imaging. 1550nm light has potential in industrial OCT applications, because it is very eye safe.
Huber and his colleagues used the FDML laser to obtain the first dense three dimensional ultra-wide-field OCT images of human retina in vivo. In ophthalmology special cameras, called fundus cameras, are used to image the interior surface of the eye. Scanning laser ophthalmoscopes can also be used. In a single shot, the Munich group’s setup achieved a 70° field of view. From the 3D OCT data, an en face fundus view can be reconstructed, which exceeds the quality of fundus cameras and is approaching that of scanning laser ophthalmoscopes.
‘Compared to our setup, commercial OCT systems capture fewer than 5 per cent of the interior surface of the eye,’ says Huber. ‘This increased coverage of the investigated area of our system will lead to improved diagnosis for the patient in the future, because the probability of missing pathologies is reduced.’
Huber and his colleagues are currently investigating the benefits of the high OCT imaging speed offered by FDML technology. They are also developing a comprehensive physical model of the FDML laser, which is as yet not theoretically fully understood.
Working with sound and light
Meanwhile, just across the German border in Austria, Wolfgang Drexler and his colleagues at the Medical University in Vienna are developing a system that combines photoacoustic tomography (PAT) with OCT.
While OCT is sensitive to scattering, PAT is sensitive to absorption. In PAT, a laser beam is used to produce ultrasound waves in a biological sample through absorption and localised thermal excitation. The degree to which a particular wavelength of light is absorbed depends on the type of tissue and, in the case of blood, on whether it is oxygenated or deoxygenated. PAT can be used in conjunction with a contrast agent, but in blood haemoglobin acts as a natural contrast agent.
Drexler and his colleagues were inspired to combine PAT with OCT when they heard about a unique transparent ultrasound sensor that has been developed by Professor Paul Beard and his group at Imperial College London in the UK. ‘Researchers at Imperial had developed a Fabry-Perot polymer film ultrasound sensor, which is highly transmissive between 600nm and 1200nm, but highly reflective between 1500 and 1700nm,’ explains Drexler.
‘This makes it possible to send two laser beams through the sensor – one for PAT and one for OCT. While PAT gives information about blood vessels, OCT gives information about tissue morphology. This makes the two techniques a perfect combination.’
Using this technique the Vienna and Imperial teams have obtained amazing 3D in vivo images of mouse skin and human skin. The images show the vasculature and the micro-morphology of the skin. Potential applications include characterising skin conditions such as tumours, vascular lesions, soft tissue damage such as burns and wounds, inflammatory conditions such as dermatitis and other superficial tissue abnormalities.
While PAT and OCT are complementary, combining them in one system was a technological challenge.
‘This technique might also be applied endoscopically in the future,’ says Drexler. ‘But that is a huge challenge. Just as the other research groups working as part of the FUN OCT project, our aim is for this combined technique to give additional information and aid in the diagnosis and treatment of a variety of conditions. For example, it could be used to perform optical biopsies, giving an answer within minutes rather than days with performance levels approaching those of histopathology.’
While the FUN OCT project is scheduled to come to an end in April, the research into functional OCT is ongoing. With the OCT ophthalmology market now mature and the cardiology market beginning to form, OCT has already overcome a major hurdle in the tough medical market – acceptance. But for many applications, OCT on its own is not enough. This is why many see combining OCT with other complementary technologies as the answer to its survival.