Lenses using graphene-based technology may hold the key to transforming medical endoscopy, research results announced last year in Australia suggest. These lenses could scale down the optical components of endoscopes and reduce their overall size, ultimately broadening the usefulness of endoscopy in clinical applications.
In addition, aspherical lenses are enabling the production of disposable endoscopes that will dramatically reduce the chances of acquiring an infection during an endoscopic procedure. Meanwhile, in the Netherlands, researchers are applying sophisticated optical and laser technology to endoscopy, potentially helping cancer surgeons identify the borders between malignant and healthy tissue more precisely.
Endoscopes allow doctors to explore inside the body and search for any abnormalities. They are designed to provide the best view while minimising discomfort felt by the patient. The majority of endoscopes take the form of a long flexible tube with a light source and miniaturised camera at one end. Bundles of fibre within the tube carry as much light towards the tip as possible. With the scene illuminated, the camera captures a stream of high resolution images that are sent as a signal back along the optical fibres to be processed by imaging software.
Endoscopes have a wide range of applications in medicine. They are used in investigative procedures to diagnose patients; for delicate keyhole surgeries to guide surgeons; and in certain cases they are fitted with surgical tools to perform operations. The functionality of an endoscope is therefore dependent on the technology that can be contained within its tip. Consequently, manufacturers are reducing the size of their optical systems to make room for integrating other components into the tip of the endoscope.
However, compromises need to be made in order to do this. Dr Stefan Beyer, manager of product development for medical applications at Berliner Glas, explained that a reduction in image quality is one of these compromises. ‘Image quality is a direct function of the numerical aperture,’ he said. ‘Therefore, the smaller the lenses used in an optical system, the less the quality. In order to compensate for this, very complex aspherical designs or software “tricks” are needed.’
In aspherical lenses, the radius of curvature varies according to the distance from the optical axis. They are preferable to spherical lenses, in many cases, as they do not suffer from ‘spherical aberration’, an effect that prevents a lens from focusing all the incoming light to a single point.
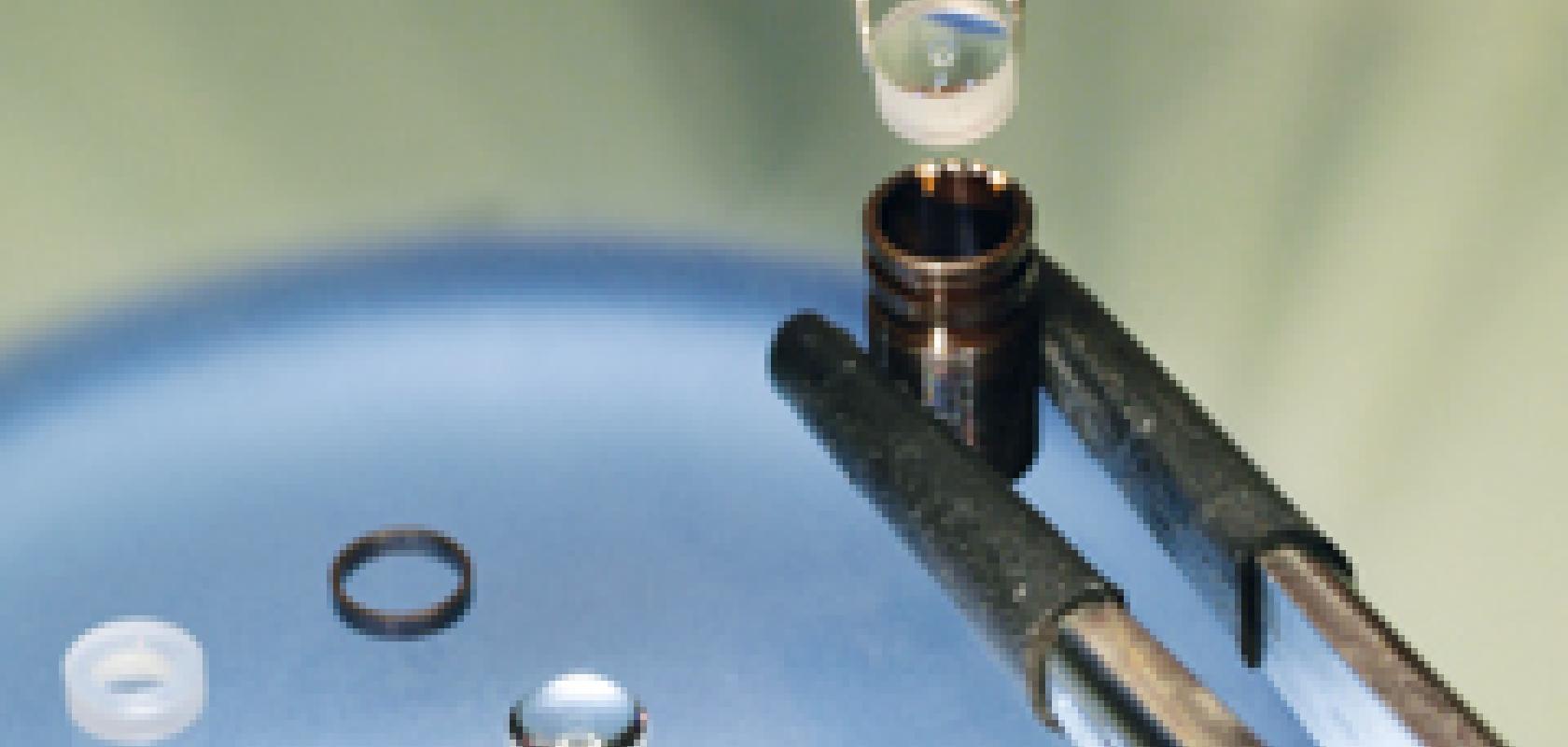
Ingo Gretschel, vice president of micro optics at Qioptiq, now part of Excelitas, highlighted the challenges in producing micro optics, even with modern production techniques. ‘There’s no new development in manufacturing that enables these smaller lenses to be made,’ explained Gretschel. ‘In order to maintain lens quality while producing extremely small lenses, we must first use larger lenses than are normally needed. These larger lenses are then centred down to the final size.’ Manufacturers are therefore limited by the production techniques currently available. However, like Beyer, Gretschel sees aspherical lenses as the route to smaller optical systems: ‘A development that would allow optical elements to be reduced in size is if aspherical lenses are used in optical systems. With an asphere, you can achieve a similar quality image as produced by a doublet lens, in addition to only requiring one element, not two or more.’
But there are drawbacks to using aspherical lenses, such as high tool and manufacturing costs. From a manufacturer’s perspective, the production of aspherical lenses is worthwhile only if the demand is great enough to push up volume. ‘This approach would become a more acceptable option when producing disposable endoscopes, as after several uses they would be replaced,’ explained Gretschel. ‘This would increase demand and therefore validate production of these endoscopes with aspherical lenses.’
Single use endoscopes are already in development; however, they are not as common in medicine as endoscopes that are repeatedly used. They act as valuable alternative, as they dramatically reduce the chances of a patient acquiring an infection through having an endoscopic procedure.
In addition to manufacturing constraints, there are also physical limitations that prevent the optics within endoscopes being miniaturised. The angular resolution of an image is diffraction-limited, which puts a restriction on the size to which an endoscope can be reduced. Beyer commented: ‘0.5mm in diameter is a reasonable estimate as to how small endoscopes can go, but with reduced image quality. To compensate for the physical diffraction limits, new ways of imaging have to be found’.
This physical diffraction limit must be overcome before optical systems can be reduced further in size. Research teams have been searching for a suitable alternative material that will allow them to ‘break’ this diffraction limit. ‘The principle has recently been demonstrated using metal-based materials – predominantly gold – but these were too inefficient and too costly to mass-produce,’ according to an announcement in January from Swinburne University of Technology, Australia.
Xiaouri Zheng, a PhD student at the Swinburne institute, attempted to produce a lens using graphene oxide. This ultra-light, transparent material is 200 times stronger than steel, while being incredibly flexible and acting as a superb conductor. The high functionality and durability of this material make it the perfect candidate for acting as a material that can break the diffraction limit. Using a 3D printer, a team at the Swinburne institute, led by associate professor Baohua Jia, was able to produce a strong and flexible lens through the use of a graphene oxide solution. Using a laser to reduce the graphene oxide, the team created three concentric rings on the surface of the lens, which created high-quality focusing properties. The resulting lens produced by the team was incredibly flat – 300 times thinner than a sheet of paper – and was able to view objects of 200nm in length, at visible and near-infrared wavelengths. Graphene-based lenses could be exactly what endoscope manufacturers are looking for in order to reduce the size of their optical systems.
With this research being only published in September 2015, these graphene-based lenses are still in the early stages of development. The research team is currently working towards integrating the lens with a fibre to create a smaller, safer and more sophisticated endoscope for non-invasive surgery.
With endoscopic optical systems already being targeted for miniaturisation via aspherical and graphene-based lensing, medical professionals could one day be using a new set of endoscopes that are able to capture high resolution images of objects only nanometres in size.
A needle in the haystack
Certain areas of medicine require a delicate approach to seeing inside the body that cannot be offered by conventional endoscopes. Whilst operating on brain tumours, surgeons must identify the borders of cancerous tissue so that they can remove the tumour without damaging the healthy tissue surrounding it. Professor Marloes Groot at the Vrije Universiteit Amsterdam is using micro-optics to develop an endoscope that is able to achieve this.
The endoscope will take the form of a handheld device that will deliver scattering photons into the brain tissue of a patient. It will be an extension of a table-top system that can scan an excised piece of brain tissue using second and third-harmonic generation, a physical phenomenon where single photons are generated via multiple interacting photons. These single photons are produced at a shorter wavelength, which allows them to scatter through the brain tissue. Scattered photons contain information about the tissue they scatter through, enabling an image of the tissue to be produced after the photons are detected by a sensitive GaAsP photomultiplier.
Groot’s team is currently using an optical parametric oscillator pumped by a Coherent titanium-sapphire laser to produce the photons required for second and third-harmonic generation. The laser operates using 200-250 femtosecond pulses at a wavelength of 1,200nm to generate photons with sufficient energy to carry out the process.
However, the laser is currently too large and expensive to be used for endoscopy, according to Groot. ‘In order to make this handheld endoscope commercially available, the laser needs to be made smaller, cheaper and easier to handle.’
This is where a compromise will have to be made in order to reduce the size of the photonic components. ‘Ideally, we would like to use a fibre laser to produce the desired wavelength; however, they are not currently available at 1,200nm,’ Groot continued. ‘One option is to use a fibre laser that produces photons at 1,560nm. There are at least two manufacturers that make these lasers, which are far smaller than our current laser.’ Groot’s team has applied for a Horizon 2020 grant with the European Union, which if successful, will be used to start developing the endoscope using a 1,560nm laser. ‘However, we are hoping a company will produce a 1,200nm fibre laser, as these are the ideal wavelength photons that we would like to use in this technique,’ Groot noted. ‘1,200nm provides the optimal penetration depth. It’s a cut off between tissue penetration and the amount of scattering.’
In order to penetrate the tissue deep enough to scatter photons off the target area, Groot’s team is attaching a needle to the handheld device. ‘A needle is the ideal way of miniaturising this set up, as we require a rigid channel to deliver the photons, not only to the surface of the tissue, but deep inside the tissue if the diameter is small enough,’ Groot explained. Currently, the table-top system can quickly scan a 0.5 x 0.5cm excised piece of tissue using an ex-vivo microscope. The system produces images in seconds, with a quality comparable to standard pathology techniques that can take several hours. ‘When I showed these images to the pathologists that we work with, they were amazed,’ Groot remarked.
In attaching the needle, however, a further compromise will have to be made in order to miniaturise the optical set-up of this system. ‘The drawback of this needle is that the field of view of the images produced is always limited. The field of view from this needle could never be larger than 300 x 300µm.’ Despite this limitation, this endoscope could be an invaluable addition to the operating room, allowing surgeons to identify tumour borders during surgery.
A graded-index (GRIN) lens is used within the device to focus incoming photons along the needle so that harmonic generation can occur at the target area. A certain fraction of photons is scattered back within the same GRIN objective, back along the needle. Groot’s team recently described their work with the table-top system in Biomedical Optics Express. ‘In the publication we show that the GRIN lens can not only be used to focus the photons strongly enough to generate a signal, but it is also efficient enough to collect the signal back in that direction,’ Groot said.
Her team has used optical components with specific material properties to produce this endoscope. Conventional optical fibres cannot be used in the device to deliver photons to the end of the needle, as third-harmonic generation will occur within the fibres themselves. Fibres with a very high threshold for these non-linear effects, so must be used in order to prevent them. ‘GRIN lenses are used as they also do not produce these non-linear effects, they are able to focus the light down the needle without unwanted third-harmonic generation,’ Groot explained. In the publication in Biomedical Optics Express, Groot’s team used a needle of 7.5mm; however they are now experimenting with lengths up to 180mm. With this optical technique working for a variety of length needles, the handheld endoscope will be adaptable to whatever needle is required to deliver the photons to the required depth.
Groot and her team could start developing the endoscope in 2017, should their application be accepted. ‘We think that the device would be ready for commercial development in 2021,’ Groot said.