In 1967, by chance, Endre Mester made a pioneering discovery about how light can help heal people. Working at Semmelweis Medical University in Hungary, he implanted tumours onto the skins of mice, and tried to cure them by shining a red 694nm ruby laser on them. Sadly, the laser was very low power, and failed to cure any tumours. But Mester noticed that the shaven areas of hair where he was shining laser light grew back faster than those on surrounding shaved skin.
Later, Mester went on to use a 632.8nm helium-neon laser to heal wounds in animals and people, said Heidi Abrahamse, from the University of Johannesburg in South Africa. He coined the term ‘laser biostimulation’, which would then go on to be called low-level laser therapy, and now photobiomodulation (PBM). The approach is now helping patients, and is evolving as it does so.
For decades, PBM practitioners believed that they had to emulate Mester by using coherent laser light, Abrahamse said. ‘But as of today, non-coherent light sources such as light emitting diodes have proved to be just as efficient as lasers in promoting photobiomodulation,’ she said. PBM is just one of several types of light medicine today – and likewise just one of those where there is a shift from lasers to LED light sources.
In general, phototherapy and photodynamic therapy using lasers and filtered lamps have been used clinically for decades, noted Kristen Maitland from Texas A&M University in the US. Light wavelengths used range from ultraviolet to near infrared, depending on the clinical application. The characteristics of the various light sources are quite different, Maitland explained: ‘Some applications require a more localised and concentrated dose of light, which is ideal for laser sources, while other applications require a more distributed large-area illumination.’
LEDs’ high-efficiency, small form factor and weight, and low cost per source are making them into a popular option for phototherapy, said Maitland. The key starting factor is a source’s irradiance, the optical power a source produces per unit area. Irradiance multiplied by time gives radiant fluence or light dose. While individual LEDs do not have high irradiance, phototherapeutic devices are constructed with arrays of LEDs to illuminate specified areas with the irradiance required for treatment, Maitland explained. ‘These arrays also allow combinations of LED wavelengths if needed for a specific application,’ she said. ‘High-power LEDs can also be used, but operating at high current creates significant heat that has to be managed, particularly if the LED is positioned close to the skin.’

Thor Biomedicine’s photobiomodulation systems use both LEDs and lasers for a variety of medical applications, including neck and back pain. Credit: Thor Biomedicine
As such, designers of LED phototherapy systems must not just achieve the required light dose for effective treatment. They must minimise time of treatment, reduce the heat released by the device, and stay below the maximum permissible light exposure on the tissue. Maitland’s Texas A&M team has therefore been working to help improve phototherapy lamp design. The researchers have developed a computational model to simulate and optimise illumination uniformity without significantly reducing irradiance on the tissue. ‘In particular, we want to evaluate strategies to diffuse the light and maximise illumination uniformity to reduce hot spots where illumination could be overly concentrated or dead spots where irradiance is insufficient for treatment,’ she said.
Understanding requirements
The Texas A&M optical model can easily simulate light distributions for different LED models or LED arrangements, Maitland continued. ‘We can also evaluate varying distances from the skin surface and materials placed between the LED and skin,’ she said. The model takes thermal management into account as a design consideration for the number of LEDs used in the array, as well as the operating current, which corresponds to the irradiance. Maitland adds that a key challenge to take into account in the design and testing of clinical devices is the range of anatomy and skin tone.
Using the computational model, Maitland’s team has designed a prototype LED array intended to inactivate antibiotic-resistant bacteria at wound sites. It consists of a flexible LED array that is placed on the skin, connected to a standalone power supply and controller. The array can conform to a patient’s body and deliver a therapeutic light dose over a relatively large area, explained Maitland. The Texas A&M scientists have already completed preliminary pre-clinical testing to evaluate how well it inactivates bacteria in animals.
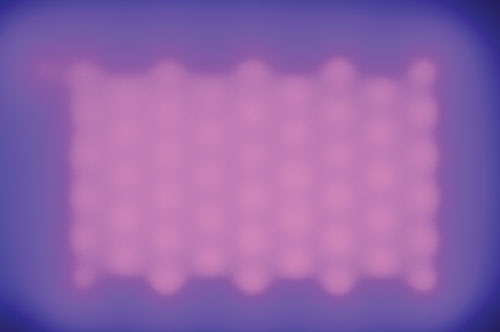
Kristen Maitland’s Texas A&M University team has used its computational model to produce an LED array that is intended to deactivate bacteria at wound sites. Credit: Kristen Maitland/Texas A&M University
Bryan Spring’s team at Northeastern University in Boston, Massachusetts, focuses on photodynamic therapy (PDT), where visible light activates drugs only in the area illuminated. The approach kills abnormal cells in skin and eye conditions and cancer. For cancer in particular, it works differently to standard chemotherapy treatment. Because it doesn’t add to chemotherapy’s toxicity, it can safely be used at the same time, Spring explained. PDT also attacks different parts of the cell to chemotherapy, meaning that it kills cancers that evade more usual treatments. ‘Photodynamic therapy is agnostic to the many classical mechanisms of drug resistance,’ Spring said. ‘It has its own class of drug resistance – it’s not magic or special sauce, it’s a nice therapy to put in the mix.’ Because of these properties, PDT will become an essential part of a physician’s arsenal of cancer treatments in the future, Spring added.
Rakuten Medical’s PDT drug Illuminox gained conditional approval to treat head and neck cancer in Japan in June 2020. Illuminox is an antibody linked to a photosensitiser, part of a field called photoimmunotherapy that is now getting a high level of interest, said Spring. Some forms of PDT use high irradiance light sources, needing the coherence provided by a laser, delivered to a patient through a fibre, he noted. Additionally, clinical lamps for PDT are too big and expensive to be practical for pre-clinical research, adds Eric Kercher, a member of Spring’s group. So in seeking to discover new PDT drugs, the Northeastern team has quite different requirements.
Better therapies
In seeking drugs, the researchers do many experiments in the small volumes offered by 24-well and 96-well plastic plates. Lasers designed for PDT can only illuminate one well at a time, making the process slow and laborious. Kercher therefore sought to use LEDs to make ‘a benchtop system that was cost-effective and versatile,’ he said. ‘You have an LED array and collimating lens above it to catch as many photons as you can. With the LED array, we can start to multiplex and really cut the plate irradiation times down.’
In principle, LED arrays also have the advantage that they can be made with modules that operate at different wavelengths. However, there were no existing commercial products available to do this. As such, Kercher developed and published a simple system with LEDs on a printed circuit board, placed on top of a heatsink. Each module only costs less than $200, and is relatively simple to make for new colours of light. ‘The cost [per wavelength] is quite cheap, compared to a laser where it’s $10,000 and then if you need a different wavelength, you need a whole new laser,’ Kercher said.
The main challenge in designing such a system is keeping it cool, due to the high powers the LEDs consume. Even with highly efficient LEDs, that high power releases a lot of heat, potentially shifting their emission spectrum, Kercher explained. The Northeastern team therefore uses water cooling in its system, which is much more efficient than fans. This allows the team to use higher-power LEDs, enabling it to do its experiments faster. Having designed a low-cost LED system for PDT experiments, the researchers may now release it as an open source kit, said Kercher.
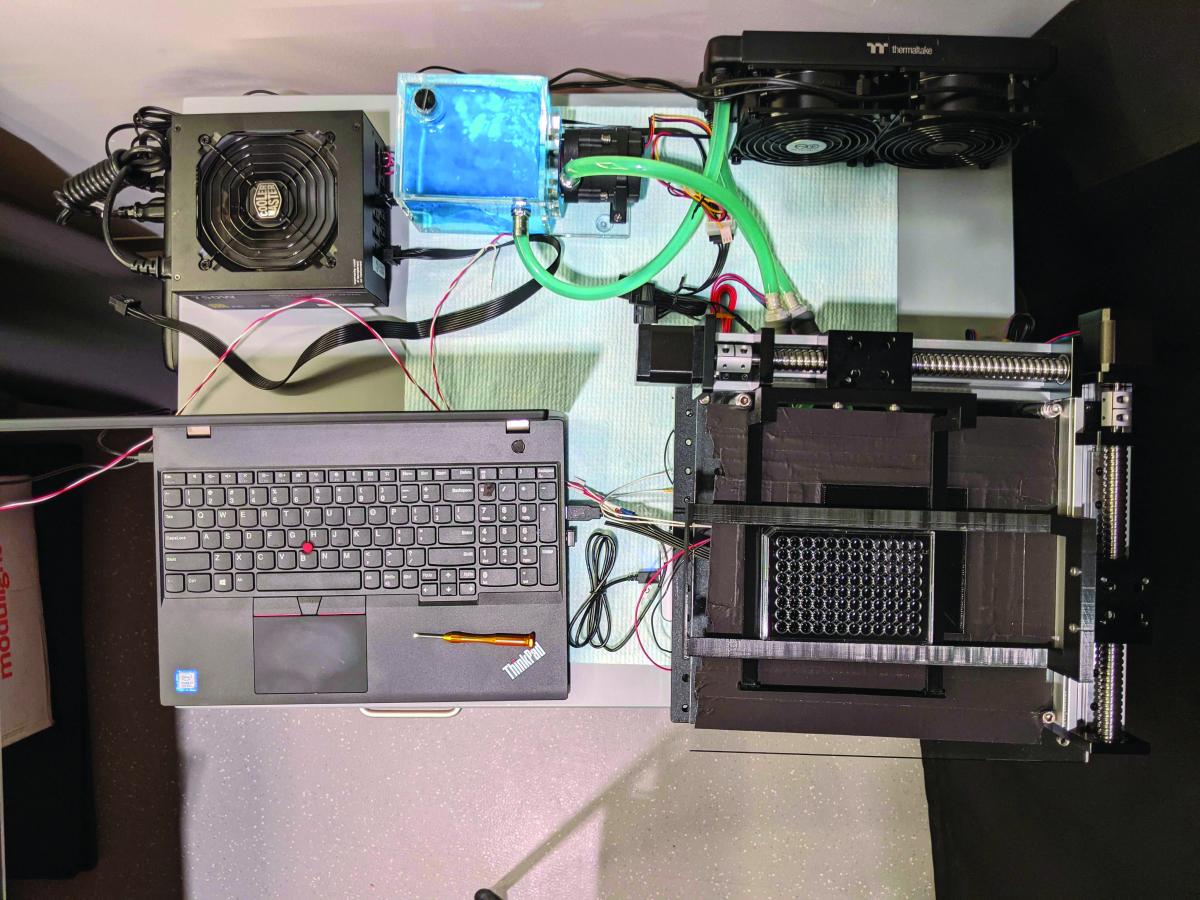
Bryan Spring’s team at Northeastern University in Boston, Massachusetts, has devised an LED array that enables experiments to develop drugs for photodynamic therapy. Credit: Eric Kercher/ Northeastern University
Unlike PDT, which works in tandem with a drug, PBM relies entirely on our body’s biochemistry, Abrahamse explained. It relies on chromophores in biological tissue, primarily thought to be in the mitochondria organelles that power our cells. These chromophores absorb light energy and convert it to biological energy, in the form of the energy molecule ATP. The energy used doesn’t have enough energy to break chemical bonds directly. Instead it excites the chromophore, enabling it to become reactive. Abrahamse said that the biochemical mechanisms underlying the positive effects are ‘incompletely understood’. ‘The complexity of rationally choosing amongst a large number of illumination parameters such as wavelength, fluence, power density, pulse structure and treatment timing has led to the publication of a number of negative studies as well as many positive ones,’ she added. However, today, there is enough evidence in PBM’s favour for it to be an established therapeutic modality.
Growing every month
The Johannesburg team’s focus is PBM for wound healing. The researchers also work on regenerative medicine that uses laser irradiation to help direct stem cells become the correct forms needed to repair diseased tissue. The research is focussed on degenerative diseases including Alzheimer’s, or traumatic brain injuries.
One key factor for the light used in PBM is that it must have a low power density. Abrahamse also noted that longer wavelength light penetrates further in biological tissue. ‘For healing superficial wounds on the surface of the skin, visible light will do,’ she said. ‘For deeper penetration, near infrared light is required.’ As such, lamps used in PBM typically span the visible to near-infrared wavelengths of the electromagnetic spectrum from around 500 to 1,200nm. The most desirable light sources would therefore be portable systems that can be tuned to different wavelengths or combinations as well as different power density outputs. ‘This would probably be possible with lasers but would be very expensive,’ Abrahamse said. While it would be easier to have different wavelengths with LEDs, it’s not so easy to have power density outputs, she added.
UK-based Thor Biomedicine provides PBM systems that use booth lasers and LEDs for this purpose. ‘We provide treatment protocols and training that teach practitioners to deliver the proper dose to the proper region of the body safely and effectively,’ commented Randall Bergsted, director of sales and marketing. ‘Our customers are medical professionals, not physicists, so they rely on us for the technical details. They expect reliability, consistency of light power and wavelength, and heat management to allow for effective treatment of their patients, which is always their number-one concern. Our equipment has been used to deliver 30 million treatments without a single reported negative side-effect.’
Wound healing on the surface of the skin is one of the main applications of PBM, but the technology has ‘already moved way beyond dermatology,’ said Bergstedt. He highlighted that one of the most widely adopted applications is the prevention and treatment of oral mucositis, a side effect of radiotherapy and chemotherapy. In the UK, there is guidance recommending the application from the National Institute for Health and Care Excellence (Nice), the government body that advises on the use of new treatments and procedures. The Multinational Association for Supportive Care in Cancer also provides guidance on oral mucosits, Bergstedt said. ‘Thor equipment is used in many hospitals for this purpose and the number grows every month,’ he explained. Thor also has CE marking, which allows medical products to be sold in Europe for relieving back pain, neck pain, tendinopathies, and joint pain. Bergstedt also notes the work being done on Alzheimer’s, and says that there is ‘very exciting work being done on fibromyalgia and Parkinson’s disease’.
Bergstedt echoes Abrahamse’s comments on the growing importance of LEDs in PBM. ‘Lasers have historically been the only option for therapies that require high power, but with advances in LED technology they are becoming a viable option,’ he said. ‘LEDs have the advantage of eliminating the need for laser safety glasses and there is virtually no difference in a therapy delivered with LEDs and lasers, if the power and wavelengths are the same.’
Optical technology has come a long way since Mester’s day, with many formats of laser and now even LEDs available as light sources.
Given the progress achieved to date, and the research being done, the two fields look set to continue advancing together, improving many lives in the process.
Fluorescence spectroscopy in the fight against cancer
Researchers have developed a spectroscopic technique they’re confident can be used during a standard lung cancer diagnostic procedure

Bronchoscopy is the standard for diagnosing lung cancer, which researchers believe could be advanced with spectroscopy
Many biomedical research applications exploit the natural fluorescence response of amino acids, the essential building blocks of all proteins. These protein fluorescence responses to light have been used for everything from pharmaceutical manufacturing to cancer treatments and even biowarfare defence. Exploring this biomedical spectroscopy niche is a dive into the deep end of cutting-edge science.
Spectroscopy is an essential technology that makes these biomedical applications possible. Avantes is the trusted choice for hundreds of researchers and original equipment manufacturers in the biomedical market.
Spectroscopy advances bronchoscopy
The standard for lung cancer detection is the use of autofluorescence bronchoscopy, an endoscopic technique of visualising the inside of the airways. A narrow probe is inserted through the patient’s mouth, into the upper bronchial tree. Autofluorescence has been shown to be far more sensitive than white light bronchoscopy in the detection of carcinomas or dysplastic lesions – however, it also has a high rate of returning false positives. Researchers at the Department of Respiratory Diseases in Rotterdam, The Netherlands have investigated the use of absorbance/reflection optical spectroscopy to improve specificity without losing sensitivity1.

Set-up
The team used a specially designed probe to feed through the 2.8mm bronchoscope channel with fibre light sources. The mucosa tissue was irradiated with a tungsten/halogen broadband white light (predecessor to the AvaLight-HAL-S-Mini) and a blue laser calibrated to 407nm introduced via fibre optics. The emission peak wavelength for autofluorescence of healthy tissue was 500nm. The resulting reflectance and fluorescence emissions were collected via a multichannel Avantes spectrometer installation equivalent to two AvaSpec-ULS2048CL-EVO’s in parallel.
Findings
An area that displays an abnormal fluorescence profile can be rapidly targeted for additional spectral measurements which can be acquired in less than one second. Diseased tissue displayed drastically lower emission intensity at shorter wavelengths compared to healthy tissues. The combined autofluorescence image and optical reflectance spectroscopy significantly improved the positive predictive value compared with autofluorescence alone without sacrificing sensitivity.
Both the excitation and fluorescence wavelengths at 407 and 500nm respectively are within the 360-600nm range in which blood is a primary absorber. This does create a challenge for this application, but not an insurmountable one. Researchers were confident that the modified bronchoscope with additional fibres was feasible to deploy during a standard bronchoscopy procedure.
The full report and findings can be found here: www.lungcancerjournal.info/article/S0169-5002(04)00305-8/fulltext
Trust Avantes for UV absorbance and fluorescence applications
Absorbance and fluorescence measurements are a key technology for many advances in biomedical technologies and dozens of other industries and applications. Avantes has been the trusted source for your high-quality spectroscopy instrumentation and systems for over 27 years and will continue to be your spectroscopy partner for decades to come.
Curious how spectroscopy can help you reveal answers by measuring all kinds of materials, in-line, at your production facility, in a lab or even in the field? Please visit our website or contact one of our technical experts, we’re happy to help you.
Reference
[1] Bard, Martin PL, et al. ‘Improving the specificity of fluorescence bronchoscopy for the analysis of neoplastic lesions of the bronchial tree by combination with optical spectroscopy: preliminary communication.’ Lung Cancer 47.1 (2005): 41-47