A three-year project that aims to design a medical tool that will dramatically lower the cost of diagnosing tuberculosis (TB) is underway. The Pocket project, which will run until October 2016, is the collaborative effort between six European partners and aims to use photonic lab-on-chip technology to build a TB test kit that costs less than €1,000.
According to the World Health Organisation, around 1.3 million people died from TB in 2012, mostly in poor regions in the developing world. Current diagnostic equipment is either too expensive to be used commonly by doctors in developing countries, or is not accurate enough to be effective. The Pocket researchers plan to test their low-cost device in hospitals in Gabon, Africa and Delhi, India, upon completion in 2016.
‘Ideally we want to have something that’s cheap and flexible, but with a much higher sensitivity that’s comparable with more complex instrumentation,’ said Wim Van Roy, local project coordinator at Belgian research institute, Imec.
Pocket is based on label-free sensing. This is simpler than the standard biosensor method of detecting TB, whereby an antibody targeted at marker proteins produced by the TB virus is combined with a second antibody with a fluorescent or enzymatic label. ‘Sometimes these assays need complex equipment – even the colorimetric equipment required to view the labelled proteins can be reasonably large,’ Van Roy said.
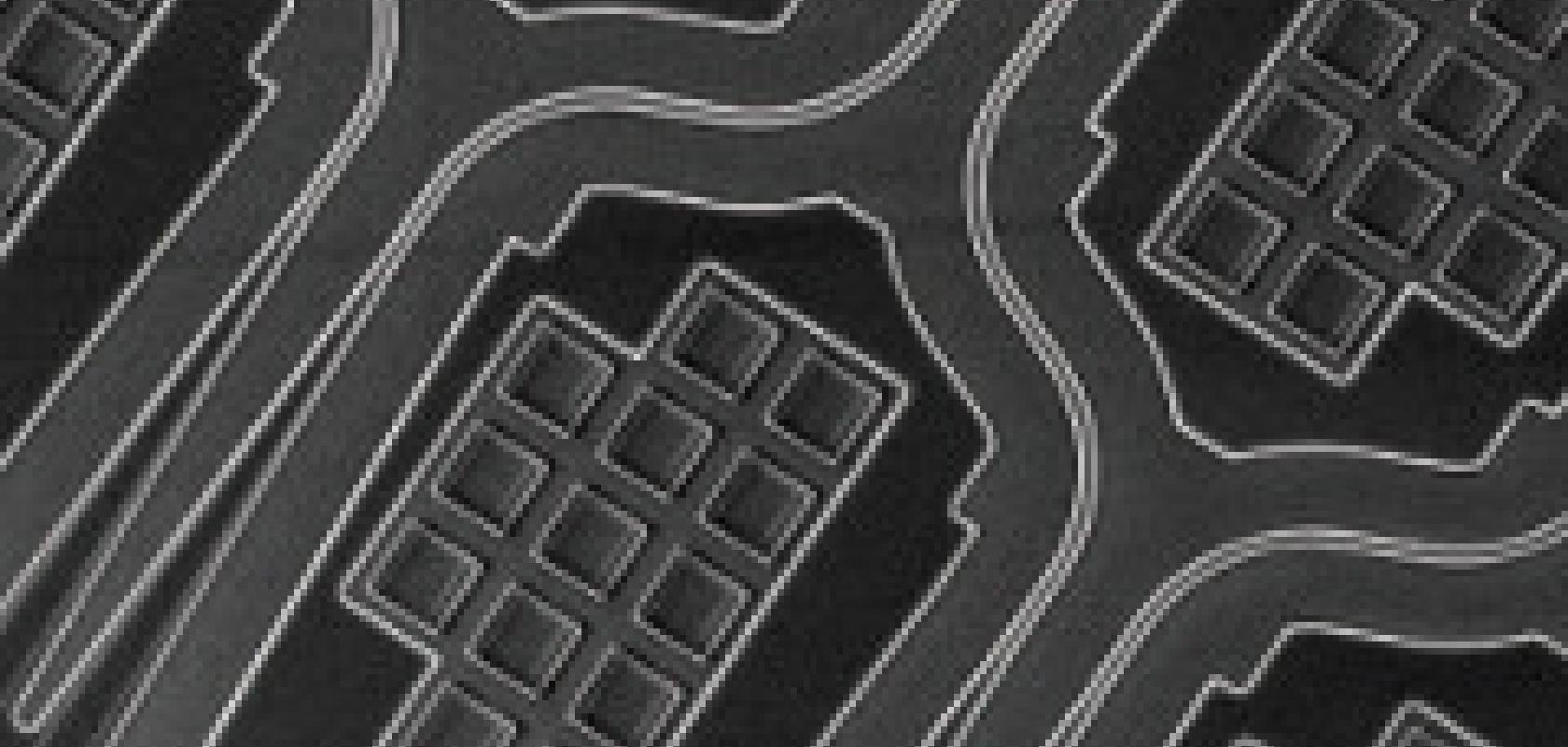
The Pocket device will detect binding of marker proteins to the first antibody directly, by sensing the change in refractive index of the medium when the binding event takes place. Waveguides etched into the top layer of silicon nitride on a silicon chip in a ring structure will act as the sensor. Part of the light will be running outside of the waveguide, creating an evanescent field. When a protein binds to the antibody on the surface of the chip, there will be a change in refractive index, which is measured.
‘This label-free detection technique essentially makes the measurement protocol much simpler,’ stated Van Roy. ‘We directly detect the binding event; we don’t have to put down the secondary antibody or the label. It’s real-time; it’s a much faster detection.’
This refractive index sensing is generally still relatively expensive, because to measure resonance changes on the order of 0.1pm requires high quality spectrometers or very fine-line tuneable lasers. However, basing the sensor on a silicon nitride chip means visible light sources can be used, which are much cheaper than the infrared lasers required for standard silicon waveguides.
‘Moving to visible light means we can no longer use silicon waveguides, because these are not transparent in the visible,’ said Van Roy. ‘So we are developing silicon nitride waveguides that are deposited on silicon substrate.
‘Silicon nitride of good optical quality that is compatible with CMOS processes is a relatively new material,’ he added. ‘The material has been only available for around one year.’
The detector on the chip uses a clever vernier cascade effect, similar to how callipers work, to amplify the signal. This results in high sensitivity, even with a white light source. The design principle is based on two detector rings with different lengths. Light passing through one ring will have constructive interference, so certain wavelengths will come through – there can be around 50 wavelengths inside the ring. Sending those wavelengths to a separate ring with a slightly different length will result in a string of wavelengths that are separated from one another.
This means a shift in resonance of 0.1pm equates to a 10pm change in the free spectral space between the pulses in the second ring. ‘We want to measure very small effects and, with this vernier principle, we really enhance the wavelength shift,’ Van Roy said. ‘Therefore, we don’t need these very high q-factor expensive tuneable lasers that can cost €20,000. Essentially, a white light source and a simple camera are sufficient to read out and distinguish the wavelength shifts.’
A lot of the building blocks for this TB lab-on-chip detector are already well-known to a certain extent. Imec has experience making the silicon ring resonators, while the overall project coordinator, Ghent University, has previous design experience with the vernier effects to increase the sensitivity of the wavelength shift. However, Van Roy commented that ‘this is the first time we’re trying to implement it in practice’.
The other partners include the Spanish research institute CSIC, which will develop the surface chemistry involved in binding the antibodies to the ring resonator. The German company Lionex has experience in producing TB antibodies and clinical tests, and the Germany firm Microfluidic ChipShop is providing its expertise on polymer microfluidics. The Flemish SME Trinean is also involved, with experience in making instruments for detecting DNA, RNA and proteins. Though this particular project looks at TB, the device could be used to detect other diseases, according to Van Roy. ‘The specificity to the target protein is through the antibody, so you can use exactly the same hardware with a different antibody and detect protein markers for other diseases.’
Early diagnosis means treatments have a much higher chance of success. Giving doctors in the developing world access to low-cost diagnostic tools could therefore reduce the mortality rate from TB and other diseases.
 Greg Blackman is the editor for Electro Optics, Imaging & Machine Vision Europe and Laser Systems Europe.
Greg Blackman is the editor for Electro Optics, Imaging & Machine Vision Europe and Laser Systems Europe.
You can contact him at greg.blackman@europascience.com or on +44 (0) 1223 275 472.
Find us on Twitter at @ElectroOptics, @IMVEurope, and @LaserSystemsMag.