From correcting vision to treating cancer, lasers have a variety of uses inside hospitals and clinics. As with any application involving a laser, rigorous attention needs to be paid to safety. However, this becomes more difficult when the user isn’t an engineer and may be performing delicate life-saving procedures.
Luckily, improved laser safety eyewear is giving doctors a better view during surgery, while better interlock systems are preventing sensitive operations from being interrupted. And, organisations such as the Laser Institute of America and the International Council on Surgical Plume are educating medical professionals about the lesser-known risks of lasers and pushing the enforcement of certain standards and regulations in clinics and hospitals.
Seeing things clearly
With a broad selection of glass, polymer and silicon protective eyewear options now available for a wide selection of wavelengths, it would seem that safety equipment manufacturers have all bases covered. According to Frank Billhardt however, head of sales and marketing at Laservision, medical customers are still on the look-out for low-weight, high visual light transmission (VLT) eyewear that can protect against a broad range of wavelengths: ‘In most cases [these characteristics are] difficult to realise in a single product. This is the general challenge for eyewear for the laser safety industry.’
High VLT eyewear is desirable in medicine, as it enables doctors to perform laser procedures with an unobstructed view. Achieving this while maintaining the required level of protection against harmful wavelengths has proven to be a challenge for manufacturers in the past.
‘Beforehand, filters which provided infrared protection also leaked over into the visible range because of the type of coating being used,’ James Saxon, technical sales engineer at Laser Components, commented. ‘When this happens, the dye may be coloured rather than translucent, which reduces the VLT. Since then, more users have been requesting a higher VLT along with the protection requirement.’

Laservision's Eyeball eyewear for patient safety
For polymer-based protective eyewear, coloured dye is essentially baked into the plastic, which gives a scratch-resistant and durable surface while providing the ability to mix multiple dyes together to protect against a broad range of wavelengths. However, certain dye colours have proven to be more challenging to achieve a high VLT with, according to Pro-Lite Technology’s sales engineer, Russell Bailey: ‘Green filters are very common for near infrared laser protection, but doctors often dislike these because they strongly obscure colour, especially red and blue,’ he said. ‘Obviously, in a surgical environment, this could potentially be dangerous.’
A light grey dye has been developed recently, which provides the same level of protection as the green dyes but with a higher VLT. This dye, which protects against Nd:YAG laser radiation at 1,064nm, is almost neutral in colour so the doctors can see better during surgery.
According to both Saxon and Bailey, progress has been made towards achieving almost transparent laser safety eyewear for certain wavelengths. ‘Companies have been developing filters that work specifically in the infrared without blocking the visible spectrum… you can now get filters that are designed for specific wavelengths and it’s like looking through glass, you would never notice the difference,’ confirmed Saxon. Bailey added that Laservision – a partner of Pro-Lite – has recently introduced novel clear polycarbonate goggles for near-infrared applications.
Laservision’s Billhardt commented that the variety of wavelengths now being used in medical applications can be a risk itself. ‘Here, the likelihood of confusion of the laser safety eyewear is a risk for the end user. Therefore, combination filters are now often requested from the laser system manufacturer to avoid this risk for the customer.’
Beam barriers
As with industrial laser systems, multiple types of physical protection are deployed in medicine to protect those in the vicinity of the laser. Unlike industrial manufacturing, however, medicine often requires that these barriers are moved between rooms and patients on a regular basis.
‘If you have a laser system set up in a hospital, say in a GP’s office, an entire area needs to be cordoned off,’ said Saxon. ‘The advantage of a laser safety curtain is it can be drawn when needed, and anyone outside the curtain won’t need eye protection.’
Laser Components offers Flexguard, a portable curtain barrier made with PT-250WB, a flexible fabric material that can block wavelengths between 190–11,100nm at a power density of 2.5MW/m2. The hinges of the barrier are coated in the same PT-250WB fabric as the rest of the curtain, allowing multiple sections to be linked together without compromising safety.
Medical applications can use a range of wavelengths the patient has to be protected from
As an extra safety measure, barrier designers have to ensure that, in the unlikely scenario of a passer by gaining line-of-sight to the cordoned off work area from outside the barrier, they won’t be at risk of injury. ‘The curtains and the barriers can have an interlock system on them as well – they have a wire coming out of them that is woven through the contacting strip, which goes between the panels or between the panels and a wall. If that’s broken the laser will turn off,’ explained Saxon.
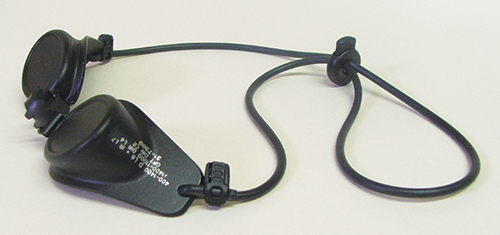
Interlock safety systems are a common feature in medical lasers, according to Bailey of Pro-Lite. ‘Medical lasers tend to have foot paddle interlocks, so a paddle needs to be pushed down to activate the laser, or an interlock where it has to be pressed against skin to activate,’ he explained. Manual interlock systems allow lasers to be switched off instantaneously without needing a free hand to do so. For operations that use a fibre to deliver a
laser beam inside the body, such as the removal of a kidney stone, this means that the laser can be switched off before the fibre is even removed from the body.
Certain medical interlock systems are automatic and have proven to be unpopular in the past, as they have the ability to disable a laser without a doctor’s permission during a delicate procedure – for example if an unauthorised person enters the operating room. Lasermet have addressed this problem through designing a maglock-based interlock system that avoids unwanted interruptions to a laser by preventing the doors of an operating room being opened whenever the laser is activated. In doing this, the safety of the doctors and patients is ensured while the integrity of the operation is maintained. Authorised personnel are still able to enter the room by using a keypad override system that deactivates the maglock without interrupting the laser.
Harmful optics
Much of the training and precautions in laser usage are shared between industry and medicine, according to Bailey. One difference between the two is medical users must be made aware of certain hazards associated with the optics used within medical lasers: ‘We’re now seeing more applications using holmium and erbium lasers for various medical procedures… they are quite far into the infrared and can use optics that are potentially quite dangerous if they go wrong.’
Bailey pointed out that lenses within lasers can degrade and become damaged over time: ‘For example, if some dirt got on a lens… the dirt could burn and cause damage to the lens itself. Once that starts happening the lens can … eventually break and shatter in the machine.’
When zinc selenide lenses start to degrade, toxic gases and dusts of hydrogen selenide, selenium dioxide and selenium are released into the surrounding atmosphere, according to Bailey. This can apparently be seen as an emission of red or white smoke and can be smelt as a garlic-like odour. ‘Anyone smelling the initial smell needs to immediately stop and put on facial protection to stop them from breathing in the fumes,’ stated Bailey. ‘It’s really about having an awareness of knowing when there is a problem and how to address the problem before continuing with a medical procedure.
‘These lenses need to be taken away and carefully disposed of. Being aware of this is part of the safety issue and something that medical laser users have to be taught.’
Pro-Lite Technology runs frequent laser training courses; the next one is 14-15 March in Cranfield, UK.
Toxic plumes
The medical practical applications seminar (MPAS) is one of the three presentation tracks of the International Laser Safety Conference (ILSC) taking place in Atlanta, USA on 20-23 March. The four-day event will cover all manner of laser safety practices, hazard-controlling methods and the latest research regarding laser safety. The conference will also play host to multiple discussions on the everyday scenarios encountered by laser safety officers (LSOs).
One of the medical seminars, ‘Laser safety: more than smoke and mirrors’, will address the topic of surgical smoke and plume, a harmful by-product that is produced when tissue is vaporised during laser surgery. Surgical plume contains carbon, cellular debris, viral particulates, toxic gases such as carbon monoxide and benzene, and a number of carcinogenic and mutagenic substances.
Patti Owens, one of the certified medical laser safety officers (MLSOs) leading the seminar, commented: ‘The latest research will be presented, analysing the toxicity of surgical plume, the impact of chronic exposure to second-hand smoke, recommended respiratory protection, new international initiatives and organisations, along with future legislation for management of this health hazard.’

Laservision's Eyelids allow doctors to access most of the face while ensuring patient safety
Owens is a member of the International Council on Surgical Plume (ICSP), a non-profit organisation committed to eliminating the risks associated with surgical plume by educating medical laser users, conducting safety research and supporting new safety standards. According to the organisation, although there are a number of standards, guidelines, and recommended professional practices currently published addressing surgical plume, they fail to have a meaningful impact due to a current lack of enforcement. The ICSP emphasises that, in order for these standards and guidelines to be enforced, they must first become legal mandates. The council believes that: ‘[A] shift to required compliance prevents staff from having to work in an at-risk environment, and patients’ safety from being jeopardised.’
Surgical plume is a hazard to both patients and anyone working in an enclosed space where a laser is being used to ablate tissue. In instances where healthcare workers have been exposed, a number of symptoms have been experienced, including burning or running eyes, coughing, sore throats, asthma, allergic reactions, nausea and headaches. These are not only harmful, but could distract a doctor in the middle of a delicate procedure.
Plume generation is a topic also currently being explored by the Laser Institute of America (LIA). ‘This is something I think that all LSOs in the medical community need to be aware of,’ commented Gus Anibarro, education director at the LIA, which regularly run MLSO training courses. According to Anibarro, The National Institute for Occupational Safety and Health has conducted studies into plume generation, which has shown that a plume extraction system should be used within two inches of the point of ablation in laser surgery.
Anibarro raised the topic of whether certified N95 filtration masks need to be worn alongside the use of a smoke evacuation system. ‘The answer to that is yes, because if you aren’t capturing all the smoke then these particulates are going to float through the air and you are going to inhale them if you are just using a standard surgical mask,’ stated Anibarro.
However, ‘the standard does not require you to use both, it requires you to do one or the other, but it prefers you to use the smoke evacuation system,’ he continued. As mentioned by the ICSP, guidelines advising the use of both smoke evacuators and filtration masks would have to become compulsory mandates to fully ensure the safety of both patients and doctors in surgical procedures.
Research centres like the Extreme Light Infrastructure (ELI) and the European XFEL being built in Hamburg, Germany, contain some of the most powerful lasers in the world, all for probing fundamental physics. Ensuring safety at these sites presents its own unique set of challenges, something that laser safety specialist Lasermet is currently working on for the European XFEL facility.
Lasermet is installing an interlock safety system for the XFEL centre. ‘In these projects, there are multiple rooms with multiple sources delivered to multiple target areas – the laser light could go to any one of those areas,’ explained Paul Tozer, managing director of Lasermet. ‘From a safety interlocking point of view, it’s a bit of a nightmare. It’s a big departure from the normal laser safety interlock situation, where there is a laser contained in a laboratory.’
Lasermet has done work in the past for the UK Atomic Weapons Establishment (AWE) where there were a number of target chambers to which the laser could be delivered.
‘With these more complicated setups, you get to a situation where you have to solve it with logic,’ Tozer said. Lasermet built its Safety Logic Plus interlock system for AWE because the organisation wouldn’t accept a software-based device.
Safety Logic Plus uses DIN rail mount logic gates, which are hardware based. The user develops a logic diagram for a safety system; there is then a physical logic gate on the DIN rail for each logic gate in the safety plan. The product conforms to the safety integrity level SIL3, and to the safety control system standard EN13849-1 at performance level E, as do all the company’s laser interlock systems.
‘The other thing that makes the design of safety systems for the ELI and European XFEL projects a safety interlocking nightmare is that you’ve got secondary radiation produced by these systems,’ said Tozer. ‘Instead of the laser radiation being a danger of serious injury, there is a danger of death. Essentially, you’re walking into a room, the laser source isn’t in that room, but if the laser source is connected to it there is danger of death. You have to have a means of detecting in a foolproof way whether the beam is going into that room, and not allow the beam to go into there until you’ve gone through a series of safety procedures.’
In the ELI project, the beam is delivered through vacuum tubes with gates and mirrors. Each of those has an interlock switch, so the safety system detects where the beam is being directed from the position of the mirrors.
‘You have to define the circumstances under which the laser is allowed to fire,’ Tozer said. ‘Because of the dangers involved you need to build up [the logic diagram] very carefully. You don’t want it to be flexible; the point is you mustn’t change it.
‘Once you get multiple rooms – say six rooms – where you could produce the laser radiation and another six experimental halls where you could deliver it, the logic is quite complex,’ he concluded.


